Claims Status Inquiry Walkthrough
Overview
Claim Status Inquiries are a very common transaction submitted in the HEALTHeNET (HeN) application.
Following is a step by step walkthrough of performing a claim status inquiry.
Quick Notes
Fidelis
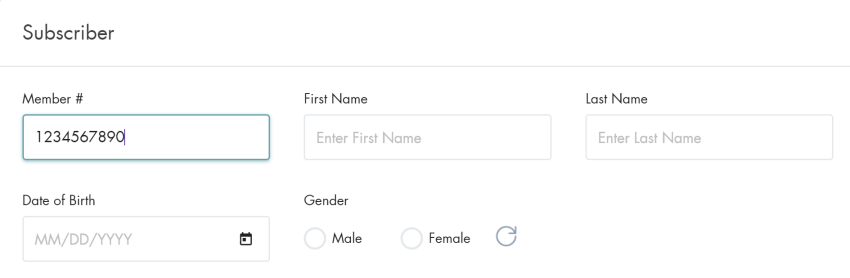
- The Member Number is required
- All submitted member data must match
Univera
- The NPI submitted must be related to the provider on the claim
- Member Number, Member First & Last Name, and DOB is required
Nova
- Member Number is required
- Member Number, First & Last Name, DOB, and Gender must match the member in the system
Additional information can be found in the Claim Status Inquiry Tip Sheet
Submitting a Simple Claim Status Inquiry
- Click on Claim Status Inquiry in the HEALTHeNET menu

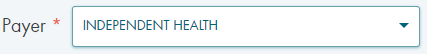
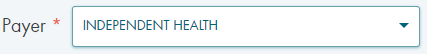
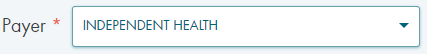
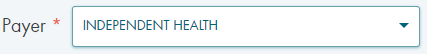
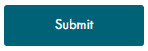
- Select the Payer from the drop-down
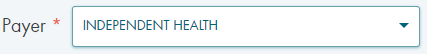
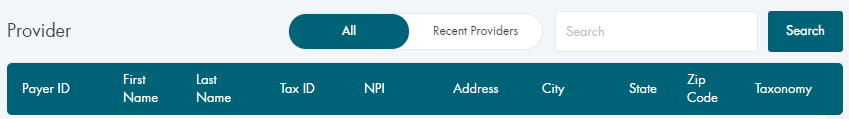
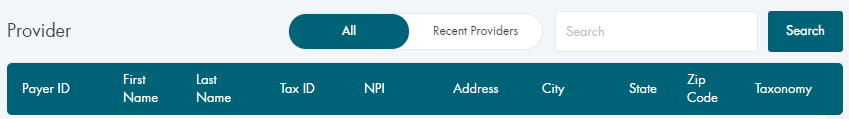
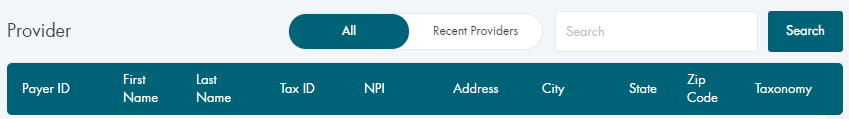
- Select the Provider
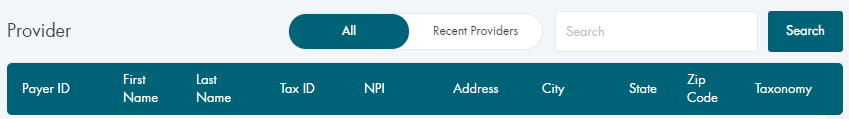
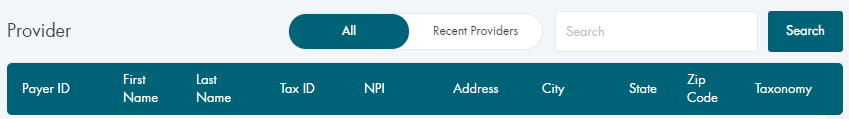
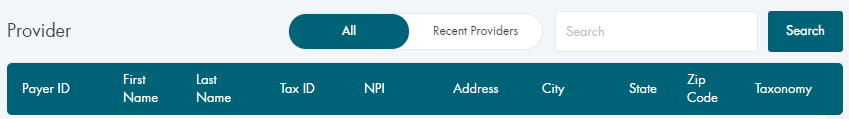
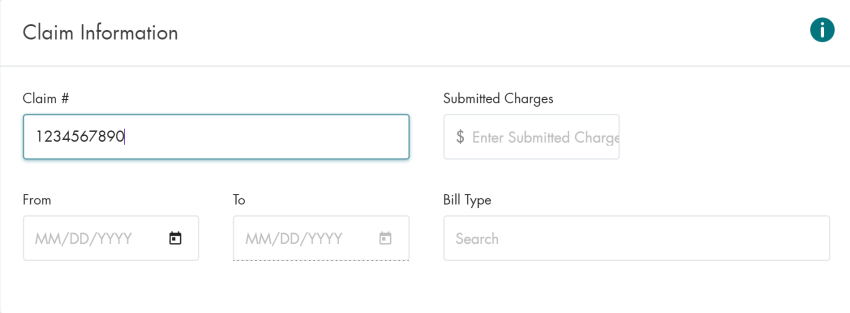
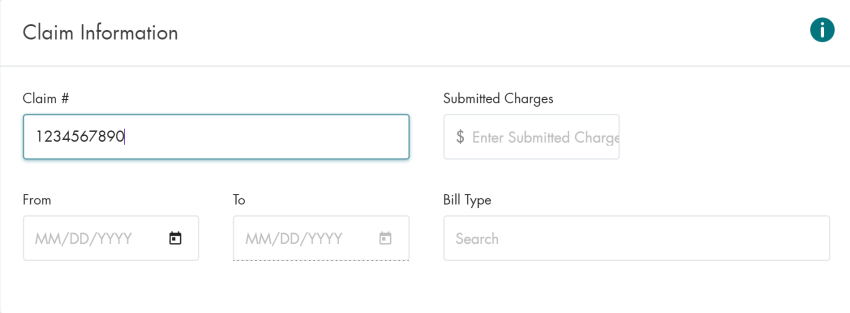
- Enter the Claim Number
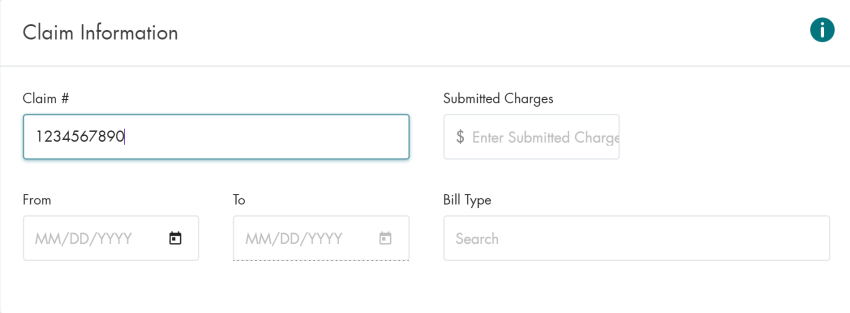
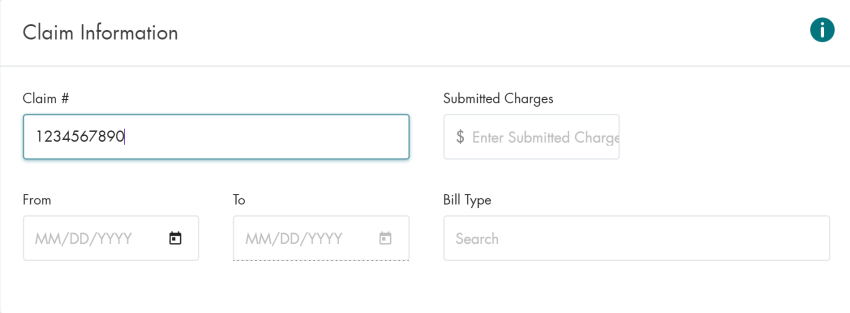
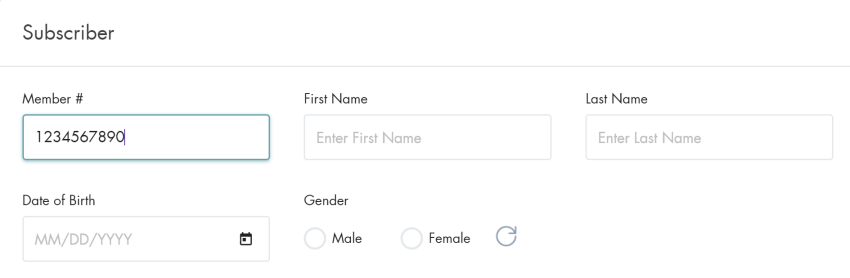
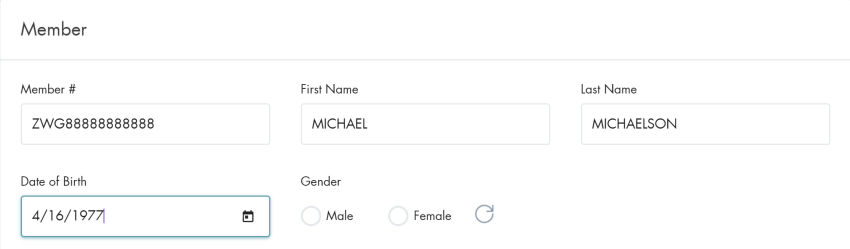
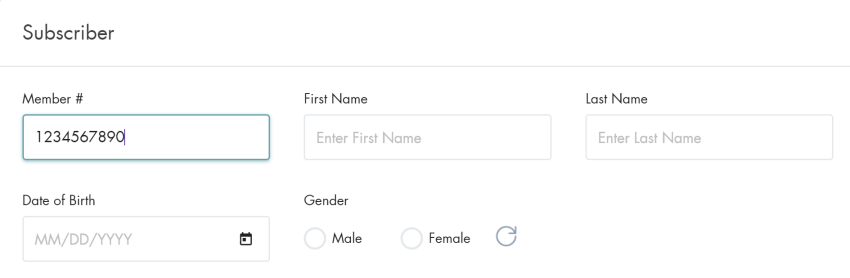
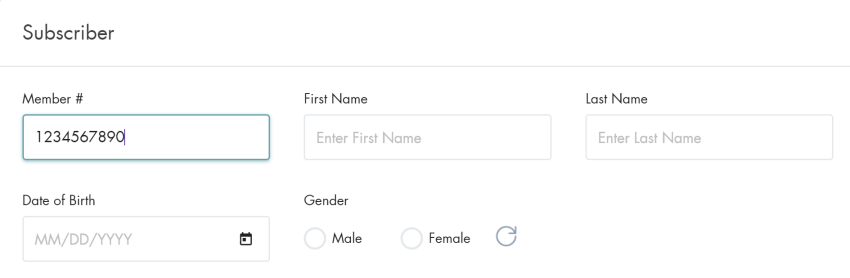
- Enter the Member Number
- Click on the SUBMIT button
Submitting a Claim Status Inquiry for a Dependent
- Click on Claim Status Inquiry in the HEALTHeNET menu

- Select the Payer from the drop-down
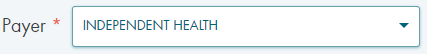
- Select the Provider
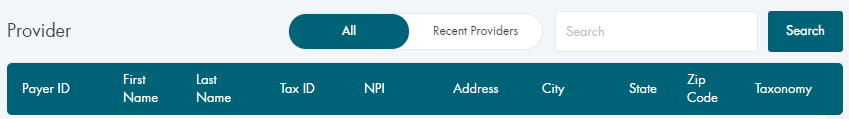
- Enter the Claim Number
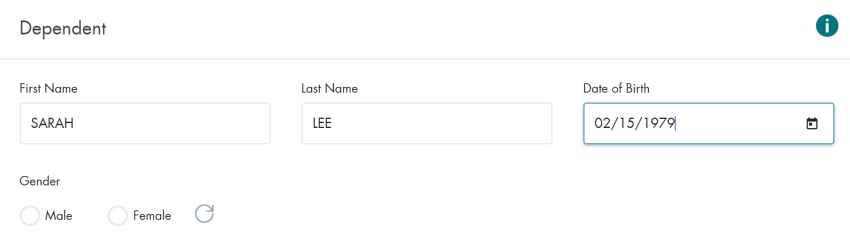
- Enter the Member Number, Dependent First & Last Name, and DOB
Note: Some payers utilize the subscriber section to accept dependent information
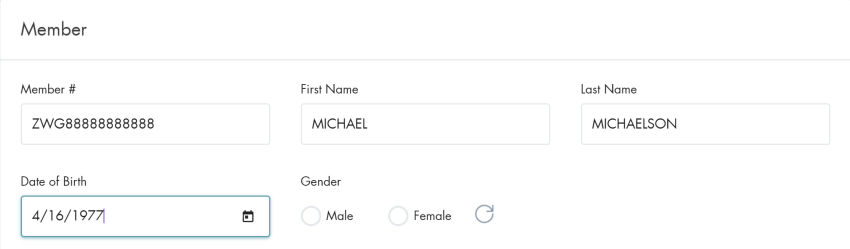
Note: Some payers have a separate section for dependent information
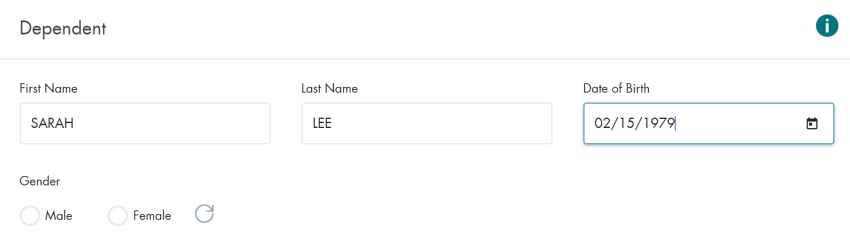
- Click on the SUBMIT button
Submitting a Claim Status Inquiry Using a Date Range
- Click on Claim Status Inquiry in the HEALTHeNET menu

- Select the Payer from the drop-down
- Select the Provider
- Enter the Date Range

- Enter the Member Number
- Click on the SUBMIT button
Conclusion
This document covers the basic use cases for the Claim Status Inquiry screen and the required fields for each.
There are additional request fields included on the inquiry screen that are either optional or required,
depending on the selected payer.