Referral Status Inquiry Walkthrough
Overview
Referral Status Inquiry allows the user to check the status of a referral request that has been submitted to a payer.
The referral request results only show for inquiries submitted to the payer through the HEALTHeNET (HeN) application.
The following is a step by step walkthrough of performing a referral status inquiry.
Quick Notes
-
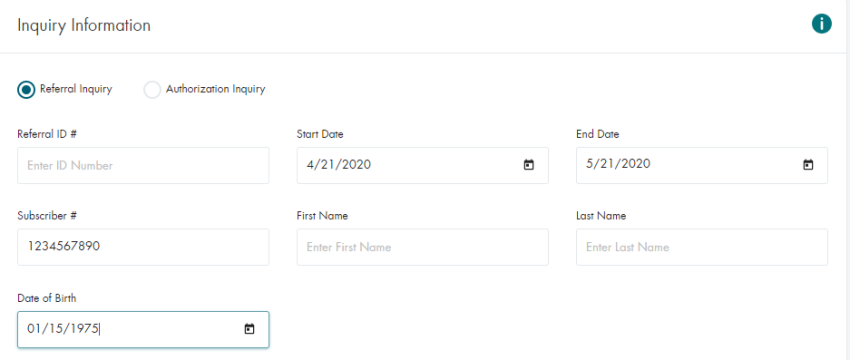
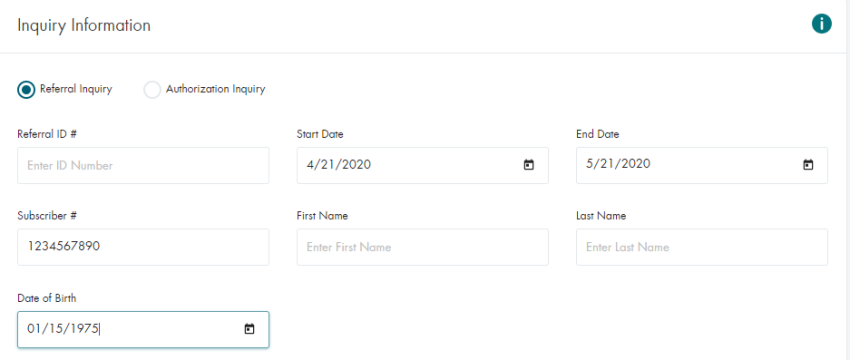
The Requesting Provider is required. This is the provider that was used when making the initial referral request.
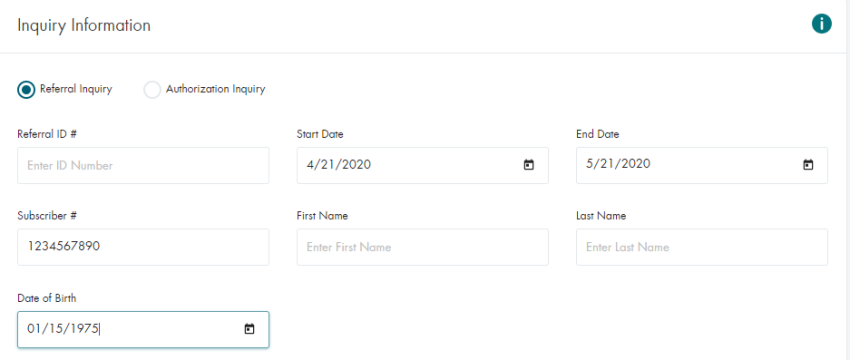
- The Member Number and DOB are required.
- Either Start & End Dates or the Referral ID are required, in addition to the member data.
-
Additional information can be found in the
Referral/Authorization Inquiry Tip Sheet
Submitting a Simple Referral Request Status Inquiry
- Click on Referral / Authorization Status Inquiry in the HEALTHeNET menu
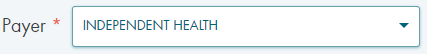
- Select the Payer from the drop-down
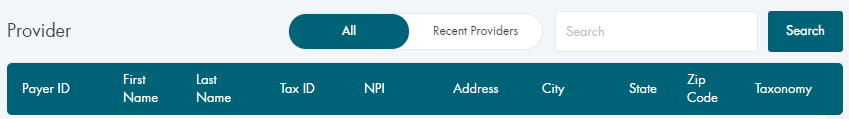
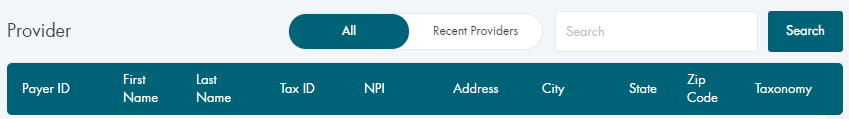
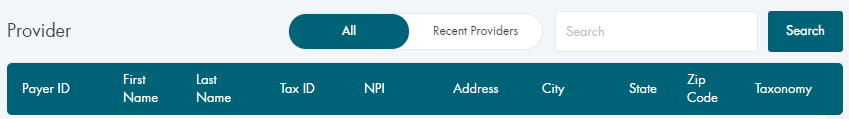
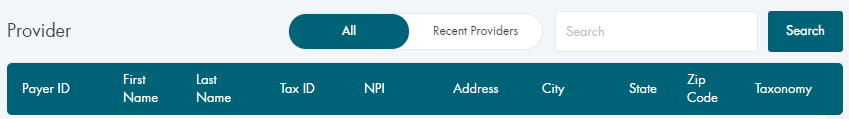
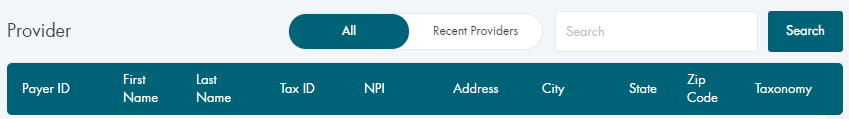
- Select the Requesting Provider
Note: The same provider that was used to submit the initial referral request.
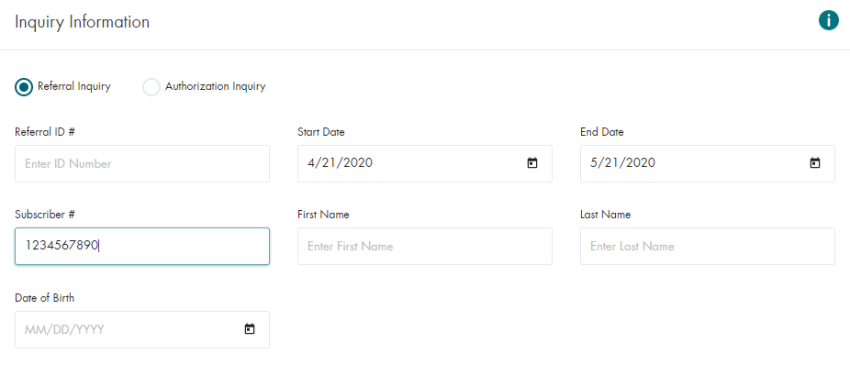
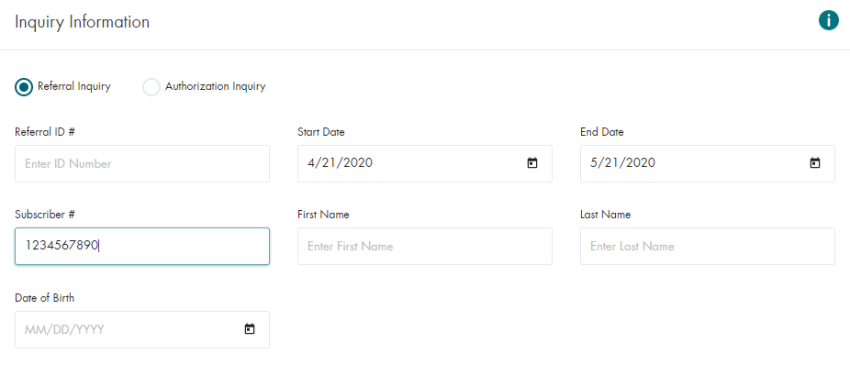
- Enter the Inquiry Information
Note: The information should match what was submitted with the initial referral request.
- Click on the SUBMIT button
Submitting a Referral Request Status Inquiry for a Dependent
- Click on Referral / Authorization Status Inquiry in the HEALTHeNET menu
- Select the Payer from the drop-down
- Select the Requesting Provider
Note: The same provider that was used to submit the initial referral request.
- Enter the Inquiry Information
Note: The information should match what was submitted with the initial referral request.
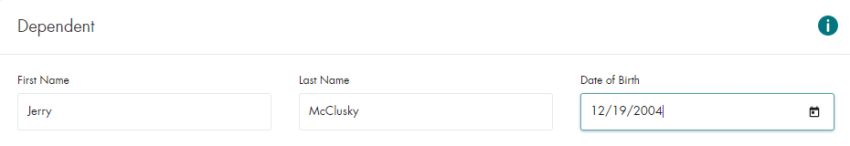
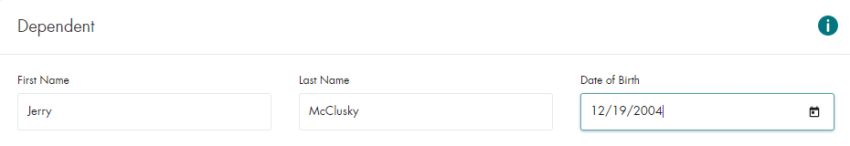
- Enter the Dependent Information
Note: The information should match what was submitted with the initial referral request.
- Click on the SUBMIT button
Conclusion
This document covers the basic use cases for the Referral Request Status Inquiry screen and the required
fields for each. There are additional request fields on the inquiry screen that can be included to assist
the payer with identifying the referral request.